Milie Fang, Writing Center Tutor Alumni Profile
9/28/21 Interview with UIC Writing Center Tutor ‘14 alumna, Milie Fang
9/28/21 Interview with UIC Writing Center Tutor ‘14 alumna, Milie Fang
- Pronouns: She/her/hers
- Graduated: BS 2014 in Biology, minor in Nutrition; Doctor of Osteopathic Medicine May 2021
- Took 222: Summer 2011 with Lydia Saravia
- Tutored: Fall 2011-May 2014 as staff tutor; April 2015-Fall 2016 as volunteer
- Now: doing 1-year broad-base residency in Chicago at Amita Health before starting 3-year Dermatology residency in Portland, OR
- Canine sidekick: Nora
So you’re back with us in Illinois now, is that right?
I know! I’m finally back after going to Indiana for med school. I don’t know if you know how the math works when you apply for residency, but I’m super happy to be back for this one year before I go to Portland, Oregon for my dermatology residency. Yeah, it just works out perfectly–so, you know, I can be home with my family here before [I move west]. I don’t know how it’s supposed to be over there, I’ve [always] just been a Midwest person, and it’ll be a new adventure, but I figure it will be the last time I’ll be able to experience something new before I settle down.
Tell me about your schooling. Where did you go after UIC, and, for people like me who are totally ignorant of the residency structure, could you say a little bit about how that stage works?
Yeah, great question. So, after UIC, I took a few years off to just make sure I wanted to do medical school and be a doctor. I really wanted to make sure it was for me because at the time I was still exploring what I wanted to do–I love design, I really enjoy writing. I was still figuring that all out, and volunteering and things like that. So I did.
That’s right–I remember you volunteered at the Lighthouse [Chicago organization serving the blind, visually impaired, disabled and Veteran communities].
I did, yeah. No, that was awesome. I also worked at UIC, in the Development Center at Taylor and Ashland [UIC’s Child and Family Development Center, dedicated to early intervention services for young children with disabilities and their families]. They had a Read Aloud program; it was through UIC’s Mental Health and Disability Alliance club. They had a Latino-American family group for kids with autism, so I volunteered doing that. [At the same time I was] doing research in the Applied Health Sciences. And I was still keeping my ties with the Writing Center–and I’m sure I did other things. I still scribed in the Emergency Room at Rush. Anyway, those years were really beneficial for me. I felt like it was really good to get some life experience before going into medicine. I found that when I went to medical school, which was at Marian University in Indianapolis, that my younger peers [who entered straight out of undergrad] were maybe a little less mature, though wonderful people. I think they were like, “Oh my god! I didn’t know med school could be this crazy.”
And I imagine it is crazy! Is it just the sheer intensity of hours you’re doing or the sheer amount of knowledge you’re stuffing in your brain or is it the culture that’s crazy? What’s crazy about it?
The crazy sheer amount of knowledge. It’s not difficult, none of the knowledge is difficult. It’s just [a problem of] shoving it in your brain and finding a way to remember it all. And so, what was sort of nice for me was that during those years off, I also tried to take the MCAT. I took it three times, because I didn’t like my score. Each time that I’d take it again, I’d be like: Well, okay, I did go up a point. But by the third time, I was like, let me actually try to learn something rather than just stuff [facts] in my brain. And I think that really shifted the way I approach medical school. I just came in [to med school with the mindset]: Let me just try to actually learn and use my logic to understand what’s going on. And then it would be easier to remember because I went through it and thought about it logically, you know, like a math problem. And [as a result] I did well on the Boards, and I realized, Wow, I could apply for Dermatology [for residency]. So anyway, after med school, then yeah, you apply for residency. And it still feels fresh to me because it’s only been a year [since applying]. And then you got a pandemic.
Anyway medical school is four years, but I took a year off between my third and fourth year to do a research fellowship at Northwestern in the Dermatology Department because I wanted to–the same thing as medical school, you know–I just wanted make sure that dermatology was for me because during med school, they’re like, “Oh, keep your mind open, explore options” but then by the end of your third year, they’re like, “Okay, you are going to have to know what you want to do because you have to apply to residencies.” [I chose to apply for the fellowship] because I had done a dermatology elective, I had support for it, and I had a lot of experience during undergrad with research, and, you know, the original reason I thought about medicine was because of my own skin problems.
Am I right that you also have–is it eczema, a little bit of that?
Yeah, yeah.
It’s in my family too.
Yeah, it’s a very prevalent problem, and, as you know, the severity ranges. So, definitely during college is when I found out how to treat it, but even then, until you get to med school, you don’t realize how little medical knowledge you have. But so I took that year to really figure out that dermatology was for me, but I also wanted to have experience in clinical research, because I’d never had that before. That was really awesome. I loved it, I mean I still like the bench research that I did at UIC. That was really fun. Like, I remember telling myself in med school, “I’m just gonna go work for Dr. Koh [who ran the lab Milie worked for as an undergrad] and I’ll just keep working at the Writing Center–I’ll find a way! I’m very happy there.” But yeah, clinical research is so awesome because you get to work directly with patients, and it feels like you’re doing something novel, all research projects are new and novel, and you know, you can kind of feel like there’s a direct benefit to patients–of course, when I’m reading the consent form, it says, “There’s no direct benefit to patients.” But you know, you’re helping research, and I think that makes them feel good about participating too. It was just everything coming together–all this hard work that had happened before. Like if it was a drug study, obviously a lot went into the development of that drug for these genetic skin problems that people had had no treatment for until then. So that was really cool. I can go into specifics on that, but that one year was amazing and I got to work with aa world-renowned pediatric dermatologist, Dr. Amy Paller, who wrote this amazing letter for me apparently. I didn’t know, because I don’t really ask, you know? I’m just like, “Whatever you think I am, just write it down!” She’s also the chair of the Dept. so she holds a lot of weight anywhere. So I was super fortunate that Northwestern took me, and then I got to work with her, of all people!
Was she a mentor for you?
Yeah yeah, for sure. I really respect her so much because of all she does. When I started there, I was like, “Oh my god, there’s 30 clinical trials on this paper [by Dr. Paller]”–you know, we have these meetings where all of us are presenting our projects, and it was like, whoa! And then she gets like 600 emails a day and replies to all those in 24 hours. I don’t know how she does it. She’s the hardest worker I’ve ever met. And so,she just showed me you can do it all if you really want to. She has her own lab too. So it’s amazing that it’s possible–especially as a woman.
She also has a clinical practice too, or was she doing more clinical research?
Yeah, she did it all. She has a lab, she does clinical research, and she does clinic, I think two to four times a month, and she would have 30 to 40 patients a day to see during those times. Yeah. Incredible. Like, do you sleep? And she’s like: Yes I sleep.
She ended up writing a recommendation for you, So do you apply for residency like you apply for a job almost?
Yeah, it’s just like applying to med school again almost. You have to get letters of rec. You can submit a maximum of four to each program that you’re interested in. But typically for dermatology, they prefer–they don’t say this, but they do–prefer three of them to be dermatologists who are academics and then the other one could be internal medicine or just another specialty, for another flavor of you in a different setting. So my fourth letter was from the Program Director for an OB GYN residency in Indianapolis. And then you have to fill out work experiences, volunteer experiences, research experiences, publications, all of that. It’s very similar to applying to med school application except that for med school apps you have to additionally write about your most meaningful experiences and pick out three–although this past year, because I’m mentoring someone who’s a DO applying to Derm which is a very hard thing to do, she told me that they introduced a supplemental application where you have to pick out significant experiences, so it sounds like it’s still very similar. You also submit your transcripts, you have to take all these exams, and as a DO, I took both exams that the MD students take [as well as those DO students take]. So I took my COMLEX for the DO boards, and I also took STEP which is for the MD boards just because I know I would regret not taking it if that was a factor in terms of choosing me over an allopathic [degree student].
Can I ask a naive question? What is a DO?
Yeah, no, it’s okay. So, DO stands for Doctor of Osteopathy. It’s a medical degree that’s very similar to MD, which stands for Medical Degree. There’s more similarities than not. You know, we can still practice medicine the same way: we can all write prescriptions, and we all follow evidence-based medicine in treatments. Then the additional part is that we get hands-on training in osteopathic manipulative medicine, where we basically use our hands as a tool to help heal the patient, and [look from at things from perspective that’s]–here’s a word you hear all the time—“holistic.” Essentially, trying to see the body, mind, and spirit as connected and always have that lens when you’re seeing someone. So for me: say it’s a rash. You’d go: Hmm, and really go into the history and understand all the stresses going on. Which allopathic people do as well. I think there’s an emphasis in terms of who founded the DO school. It dates to I think 1891 , when the founder [Dr. Still] opened the first school of osteopathic medicine in Kirksville, Missouri. Yeah, there’s a lot of history. It’s really wonderful. I didn’t know too much at the beginning about osteopathy, but I just liked the philosophy. But then, we have clubs at medical schools. I attended a lot of the ones where you can get more practice doing OMM (osteopathic manipulative medicine). . . And I thought that was really powerful, just seeing how things are connected. So, you know, I started seeing an osteopath this past year because of neck pain. And I go in to him and he’s like, Oh, it’s because your right wrist is so locked up. He fixed up my wrist and then my neck pain just melted away!
Is a DO something that everyone in med school has the option to pursue or is it an either-or choice, where at some point you have to decide, DO or MD?
A: I think most med students go to MD school. Though this doesn’t apply to all, I think some people might have biases towards one and just won’t even bother applying to the other options but, for example, there’s MD schools you can apply to; there’s DO schools you can apply to; there’s Caribbean schools and international medical schools you can apply to. So, there’s a lot of options to get from A to B. And depending what specialty you want to do, it is more challenging as a DO, Caribbean or an international medical student, but it’s not impossible. I know plenty of people that have come from an international program or Caribbean program that have matched (for a residency) and been super happy. But yeah, it’s definitely a struggle to get in, just because there’s not enough residency spots, depending on your specialty. And I think, at the end of the day, you just have to be really motivated. And so if you really want to be a doctor, if you apply and you don’t get into allopathic school, you don’t get into osteopathic school, [there are options]–you don’t have to give up on your dream. I think everyone has their own breaking point, I guess, before they decide, let me go on a parallel path. For example, for me: If I didn’t get into med school, I’d be very happy being a research tech or lab manager.
That’s good to hear that there’s a lot of different paths and everyone has to calibrate for themselves how much they want to pursue medicine and at what cost. Was your school, Marian U. in Indiana, a hybrid DO/MD program? I know you chose to take the DO and the MD exam or did I misunderstand that part?
Yeah, my school is an osteopathic school. It’s also the [first medical school in Indiana in 110 years]. They’re proud of that too. And in terms of me choosing electively to take the MD boards, you don’t have to at a DO school. I did hear some DO schools require you to take both. But for me it was elective. I knew that dermatology is very competitive, and that just a very, very, small, tiny percentage of DOs match into dermatology, and so I wanted to think about my audience in terms of when I’m applying: what would help them compare me. And the two scoring systems for the two exams are very different. So I just went ahead and took both exams. I took the one that I needed to graduate medical school, which is the DO one. And then, for the allopathic one, the MD exam, it was just easier for the admissions people to compare me one-to-one with my allopathic peers [if I took it too]. Because I think that’s the big concern of MD programs. Unfortunately, a lot of people don’t know what the DO is. And there’s been bad press. Of course, for MDs too, but you know what an MD might look at the DO, and say, Oh no! They’re all quacks.
That makes a lot more sense to me! I didn’t realize that your school was an osteopathic school but you electively chose to take the MD exam so your score would be a little more legible to admissions when you applied for a dermatology residency. I understand now.
Yeah, yeah, exactly. And it shouldn’t be that way because now, you know, there’s a single accreditation; there used to be two different matches, but then they combined it in the year 2020. But, you know, I think, just like battling systemic racism, things are just gonna take some time, when it comes to like prejudice and discrimination. So I’m really thankful that hopefully I can be like a mentor/example of us [DOs] breaking that barrier because I matched into an allopathic program [for residency] and, it has happened in the past, but, you know, not, I would say, enough.
And so that idea of matching from an osteopathic program into an allopathic residency is sort of crossing a glass ceiling between two divisions of medicine a little bit?
Yeah. It feels that way, at least. So yeah, I was thrilled. I’m happy to show you my match day video!
I hadn’t heard that term before, “match day.” Is that something that everybody has on the same day and compares where they got in? Is that a thing?
Yes, so you’ll have like match week, where the Monday you find out if you matched at all. And if you didn’t match, which does happen, you can enter the SOAP, “supplemental something application.” So basically, any spots that residencies weren’t able to fill are open for people that were not able to match into residencies: they can find each other, almost? There’s a process to do it, but it’s done in a way so that by Friday, match day, you can join your peers to celebrate and hopefully match somewhere. But not everyone wants to do this, especially if they want to do a competitive specialty, like dermatology, they might decide not to participate in that and try again the following year. But yeah, that’s match day, Friday, where traditionally, everyone goes to the podium and they open the envelope and say where they’re going, which is really nerve racking, I wouldn’t want to do that! What my school did they did was an option where you could do it at home with your loved ones because of COVID. You know, they wanted to limit how many people are in the room. So I just did at home with my husband, and I was like: Oh my god, they sent it! I’m clicking it now!
And was dermatology your first choice? I assume it was the specialty you had applied for primarily?
I decided not to dual apply, but that is a common suggestion from medical schools to do that because it’s just so hard to get into, but I’m just so committed that like, if I don’t get in, for whatever reason, I’ll try again.
That sounds like a really huge coup for you, Milie–like your hard work really paid! Congratulations!
Yeah, it’s crazy. I think up until match day, like I just didn’t ever believe it could happen. So the fact that it happened–I’m like, wow, you know like all those times, I doubted myself, I couldn’t see the light at the end of the tunnel. I was always in the mindset of, like, who knows, it’s so hard—-even the best people don’t match in dermatology.
Is dermatology one of the most competitive specialties?
Right, yeah, it is. Year after year, dermatology stays ranked as the most competitive specialty. But to go back the training part, to finish about a thought about the road to get here–it has been an amazing challenge, definitely worth all that pain and struggle. You know, even if I hadn’t matched, you know, I’d still just be thankful for all these experiences I had up until then. But yeah, once you get a residency: Dermatology is special where you have to do a one-year broad-base education first, like, into, internal medicine; I did ICU the past few months (wow, let me tell you, that was crazy!); you have to do general surgery; emergency medicine. It’s almost like a repeat of your third and fourth year, but you’re now paid, you’re a doctor, you can put your own orders and things like that. So, yes, you have to do a broad-base year, and then after that, you can go into your specialty for three years. So after this year I’ll do three years of dermatology and then after that if I want, I can do fellowship etc. The other specialties that are like dermatology are radiology–they also have to do a broad base year– anesthesiology, ophthalmology, physical medicine and rehabilitation. And those are the ones I can name off the top of my head. Then the rest–family medicine, internal medicine, pediatrics etc.–they just go straight into their specialty. Versus me, in addition to applying to dermatology, I had to apply separately to these one-year experiences.
So this year in Illinois at Amita Health is where you’re doing that kind of whirlwind internal/ICU/ER broad-base experience. That’s the transitional year, and then you’ll move to Portland for the three-year specialty.
Yes! That is accurate.
Are you getting paid this year then?
Yes, it’s my first salary, ever!
Great! And have you started–you’re at Amita full-time, is that right?
Yes, that is correct. Almost all residencies start July 1. But ours starts a week before, since they know we’re just here for the year, so they give us an extra week for the following year to move to, our other locations. Which is great since I have to move to Portland. I was going to go by plane, but then I found out my dog doesn’t fit in those carriers under the seat. So I’m gonna drive there.
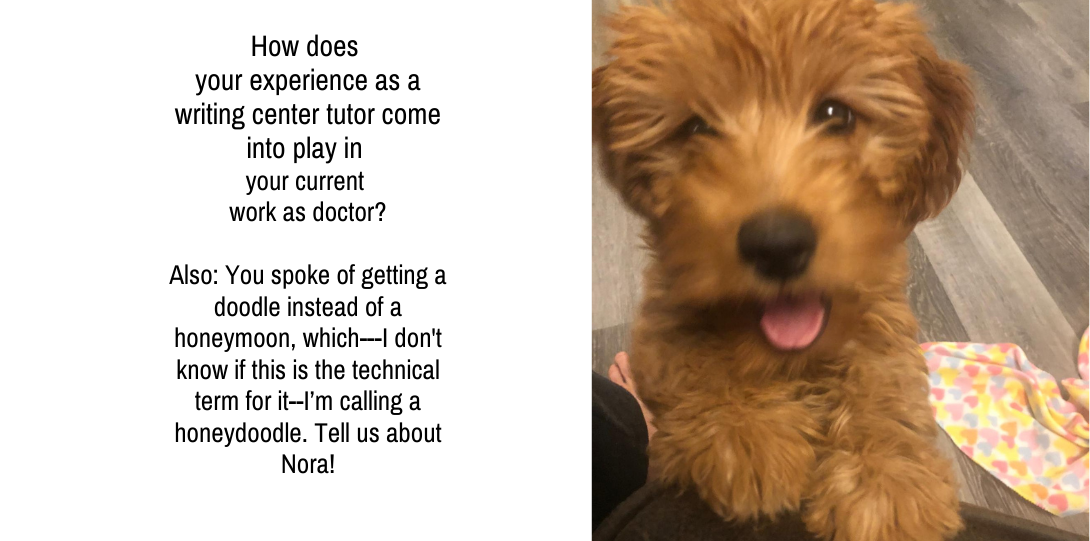
You have a doodle? Am I right about this? You spoke of getting a doodle instead of a honeymoon, which—I don’t know if this is the technical term for it–I’m calling a honeydoodle.
Yeah! Honeydoodle. Let me go get her. Nora! Meet me friend, Kim.
[I ask permission to take a screenshot.]
She turned six months last Sunday so she got her spay surgery. That’s why she has the doughnut. She liked the doughnut much better than the cone.
And is she at her full size and girth?
I think at one year, so right now, she’s half–she’s 16 pounds. And we got her when she was five pounds (great day!). And she’ll get to, like, 30 pounds.
That is so exciting. When did you get her? Was this right after you got your news on match day?
I wanted to, but then, you know, we were planning our wedding for a while, so May 30 was our wedding, and I just knew if we got a puppy, that would just add more stress. So we got her immediately after we got married though.
So you, you had this fast succession of major life events: you got matched, you got married, you got doodled, boom, boom, boom.
And then we had a move here.
And when you moved here from Indiana, was your partner in Indiana too?
Yeah, he came me with me the whole time. When I found out about med school, way back when, I was like, Are you gonna come with me or. . . ? And he was like, “I’m coming with you!” And so he came with me. Then moving back here, he came with me too. Luckily, his job is remote now, which is awesome, because otherwise I wouldn’t agree to this adorable dog, because I’m like–I won’t be around, I’m in residency and dogs need love and attention. So then for Portland, yeah, he’ll come with me too, since his job is, as I said, remote.
You mentioned a little bit about the road to get here and challenges. And I feel like that’s probably something current students will relate to a lot, and I was curious to hear your reflection thinking back. What were some of the points that were the most challenging, and how did you get through them? Or, thinking back on it, is there advice you would have wanted to give your past self in those moments to help you get through?
I recently gave advice to my aunt’s kid, in high school. And I think my big advice for her was: if you get a B in your class, a C in your class, say you even failed the class, that is NOT the end of the world. You could still do it. And, you know, don’t listen to the naysayers because that’s where you’ll doubt yourself. And I think, for me, my biggest challenge has been believing in myself and having confidence. And so, I also learned during med school, I would say my first year, yeah, I didn’t know, I had depression. But it was really bad. I had no idea. And like mental health is, you know, really taboo subject, just growing up in an Asian household. And so, I just had no idea until like, at one point I was crying every day for nine days straight and I couldn’t study. It was just weird because I had never not been able to study before. And so, I thought: I need help. And luckily the school is really great. I’m guessing, I’m hoping, most medical schools are too, but our med school always sends us these messages like: hey, like if you’re struggling like we have a counseling center right here it’s a free service for guys. So, yeah, I think that was a huge, huge thing for me to do. . . I think a lot of people when you have not like had that experience of like . . I mean I’ve had experiences of being sad and stuff but I didn’t realize it was a problem? And that it affected me negatively. And so when I got professional help, it almost felt like I was giving up on myself that I need this, but really it’s like no–it’s taking care of myself. And so the concept of taking care of myself, I did not learn until Medical School, which is a real shame. I wish I had learned it earlier in college. Like, I wish I had gone to the Counseling Center–though it was a far walk, but I wish I did that. Now, I’m like, Wow, what a change that probably could have been, and I wouldn’t have been so crazy–because, I don’t know if you remember, I was crazy. In undergrad I was working like eight jobs in one semester one time, or like, I would work 18 hours a day. That’s not healthy.
At the time I thought this is what it takes in med school; I felt like I have to do it this way because this is what they’re looking for, and this is just the sacrifice you have to make. And in med school, then, it gets even harder and then you realize you can study forever and you’re still not going to know everything. And I think once I learned that, then the shift [happened[ of like: I’m just gonna learn what I can and do my very best, because that’s all anyone can ever ask for. So I think seeing a therapist is super helpful. I’m still seeing one and it’s immensely helpful, and once I started going I was like, Whoa–everyone needs to go. It’s the best thing ever! And when I finally went, it wasn’t as scary as I thought it was. Until you are doing it yourself and are in it, I think you don’t realize how many other people are having problems [too]. And so it was reassuring when I went in the waiting room and I’d see classmates, and I was like, Wow. To me, it felt like [everyone else had it], totally going on. In med school I was thinking like, Oh my god, everyone’s studying but me right now, I need to go study. And then you realize that people are normal people, and they’re watching Netflix too, and enjoying their lives and working out. And you’re like, Oh, why did I have that image in my head?
It’s really interesting because it’s almost like you have this narrative that the standard is so high–there’s such a superhuman standard that you have to work yourself to the point of exhaustion just to keep up. But you’re probably actually so isolated from other people because you’re studying and working so hard that the standard is completely invented by you. I’m really glad to hear that med school culture did support seeking help, like they kind of normalized it and made it seem like this will help you in your endeavors here.
Yeah, I think because it’s just so prevalent. Like there was a campaign of #400. Four hundred physicians take their lives every year, that’s a national suicide statistic. [At Marian], they always tried to really encourage us to take care of ourselves. You think that school is just about studying all the time, but life stuff is so important, staying grounded, doing your hobbies, things like that. I had no idea. I wish I knew that before. I felt like maybe I gave up a little bit of that in college to do a lot of service. And I’m prone to saying yes to everything. And so I had to learn in med school, that when I do say yes to something it’s also saying no to something else. That helped me to cool it–like, I don’t have to reply to this email right away, no one’s gonna die if I don’t reply. And so yeah, I think just small little changes in mindset really helped me to be a more cool, calm, collected person. And during the COVID pandemic, I think things are just more fragile these days with everyone. Everyone’s feeling so many things all the time, and I’m just always thankful for my life. Like, I don’t know. I even recently wrote my own eulogy because I felt I need to know: what is my end goal? Because if you have the end in mind or the destination, you’ll know how to proceed or live your life with value. So, that was a fun exercise to do.
Was this an assignment you gave yourself or was it a therapist’s suggestion?
I gave it to myself. Unfortunately, my beautiful grandma, she was 98–we could only see her over FaceTime when she passed away from COVID at a nursing home around Christmas time. So I think around that time was just very emotional.
And then I was also applying for dermatology residencies, getting all these interviews. And to prepare for the interviews, you’re given practice questions. I think one was: “You’re dead. What will family and friends say about you?” It kind of put things in perspective. I think during the pandemic a lot of people were forced to reflect on the question: what is a life well-lived? You realize then things you regret not doing, and you go and do those things. That was part of my COVID processing, I guess.
And you know, I also saw a lot of death that year, in medicine. I went through my first code where this woman just came in [to the hospital] and something was not right. And to be honest, she was close to my age, and suddenly she just became unresponsive. And the worst part was she didn’t make it, and she had just got married to her husband. And I saw autopsies for the first time because I worked with a trauma surgeon and then they had me rotate within forensic pathology. And three patients’ died from drowning, one of them was a child, and I’m just like: medicine is terrible. I don’t know why anyone would want to do this.
So I think, yeah experiencing a lot of death just puts everything into perspective. So, yeah, that sounds like a really intense year.
Was the young woman a COVID patient?
We suspected, but all that information is on a need-to-know basis. She was my first death. But now there’s a kid with a migraine I had to go see, because you still have to go see people, and unfortunately there wasn’t a debrief after. Though I saw a nurse after and said it was my first code. I asked, Is it normally that traumatic? No, he said–I’ve been in the ER for so many years, and normally you know when someone is about to code–they’re frail. But she was so young, no medical problems–that’s unusual.
Then I was in ICU these past 2 months,, which I’ve never done in med school. So that was quite a learning curve. But they said I was the best team member they ever had. I said thanks, you’re just stroking my ego.
I think you’ve got to take it.
(Laughs) Let’s just say, I’m flattered, I guess? But yeah, in there, you see tons of COVID, a lot unvaccinated, a lot who end up dying or on a ventilator forever. It’s just so sad–and it doesn’t have to be this way. I remember I read the book The Power of Now. [The author] says that when you you complain, you are in denial. So anytime, if I find myself complaining about whatever the present is, I I think it just means I’m in denial and I need to just accept reality. You know, it is what it is and all you can do is protect yourself and try to be a role model. We can’t change others, we can only change ourselves.
It sounds like you found a couple books to guide you, in addition to a therapist and a mentor. Are there other books or podcasts or media you recommend to people that you feel like helped you cope with just the sheer volume of like trauma and grief that is part of being a med student in these in these times?
I love the Marie Kondo book, The Life-changing Magic of Tidying Up. I read it after my first year. I read so many books–I couldn’t believe how many audiobooks I went through.
I think it was because I was struggling with insomnia, and talking to my therapist about it, and they recommended I play an audiobook to help fall asleep, but not something too interesting that keeps you awake. Although I ended up just getting the interesting ones–I’m like. I don’t want to waste my time! But definitely, yeah, that one was awesome because I think, prior to med school, what I realized is that I was actually depressed in high school and probably even before that. And I just didn’t know. When you’re in medical school, you become a hypochondriac: you’re like, oh my god, I have this habit. You diagnose yourself with all these diseases. And so I think that it helped to just go through whatever was holding me back prior to med school, by going through my possessions. Like, you know–what really brings you joy? So that’s a fantastic book.
The Power of Now is a fantastic book too, because you just accept things, and you try not to judge. It helped with understanding how meditation works.
Oh, and doing yoga was really helpful during med school. Now I’m always on “Yoga with Adriene” YouTube channel. I’ll just pick one. Like, yesterday I was stressed, and I was judging myself, and I’m like, I need something, and I was like, I’m doing that video. I love all her videos, and she’s just very likable.
I read Barack Obama’s book recently. I think that one just made me realize how much I don’t want to be invested in social media. So before I took my first set of boards between my second and third year, I had removed myself from Facebook; I still have Twitter and LinkedIn, but I don’t really update them. I think Facebook was the biggest one. I realized how bad it was for mental health. Like, literally. I remember going there only for dog and cat videos. The rest, I’m just like–I don’t want to know about your happy life, I’m very busy. But yeah, reading his book, learning about all the fake news about him and what it did to his family. . . .all these things were like, Wow, thank you for putting yourself out there and being like a martyr for change. Like, that really takes a toll on a person. He earned all his white hair!
Let me see if there’s any other ones that got to me. . . Oh, this is really good: Skin Deep: The Mind Body Program for Healthy Skin. I found a free PDF online when I was realizing that my depression was also related to my skin problem, because it wasn’t getting better. I realized I just wasn’t taking care of myself. So, that book really goes into psychology of skin.
I read Michelle Obama’s book and it made me cry. But I don’t know if the biographies I’ve read have been life changing. It’s just nice to hear what other people struggled with, and to realize, you know, you’re not so different from them.
Oh, I love, The Book of Joy by the Dalai Lama. That was really great. At the time, I was doing intermittent fasting when I read that book, and I was not eating, two days of the week, which, of course. my parents would not approve. But I was by myself and I’m like. I’m doing this. And then I realized it made me feel better in so many ways. I was sleeping better, my skin was getting better, you know, I was saving money because I didn’t have to spend so much on food, I was saving time because I didn’t have to think about what I was going to eat. And then when I read the book, I was like, wow, it’s also about solidarity because they do it by choice for a religious practice, just to being reminded of what hunger feels like and that there are other people out there who are not so fortunate to have food readily available. So it’s about being in solidarity with that–that was a nice added spiritual benefit to fasting. But at that time, I went back home for that Northwestern fellowship and my parents were like, Why aren’t you eating? I can understand, as a parent, you don’t want to see your child not eat, so: fair enough. But it was really great.When I think about the the evolution of human beings in the past 60 plus years, there has so much [change in our food system] which is not our natural physiology and [which][ our bodies aren’t adapted to, which leads to so much obesity and cardiovascular disease. I’m sure there’s probably evidence-based papers published, but anyway there’s just me thinking on a personal experience about what makes sense. Your body needs to detox and have a break. So anyway. I really loved it. But I think at some point I would like to be pregnant and you can’t be fasting when you’re pregnant, so I don’t want to get used to that.
[via email:Just thought of some other books I thought were fantastic!]
I plan to read this at least 2 more times before I have children; relatable even if you don’t have children though.
- Educated by Tara Westover.
- How to be An Anti-Racist by Ibram X. Kendi.
- Atomic Habits by James Clear.
- Smarter, Faster, Better by Charles Duhigg
I think it was this book [by Duhigg] that finally got me to write up a paper where instead of “write psoriasis paper” on my calendar, I changed it to “help kids with psoriasis” and I wrote it within 4 hours (vs. dragging my feet on the idea of writing a paper for months on end).
Your choice to go into dermatology seems very personal in a way. It feels like you have an understanding from your osteopathic training of how skin is tied to overall health, both mental and physical, but you’ve also had firsthand experiences with how your skin was connected to your overall well-being. Would you say that’s the case, that dermatology is a choice that gives you a chance to think about some of these philosophies that you’ve come to understand about health as a relationship of mind, body, and spirit?
Actually I think I feel like, as someone who struggled with [skin issues] and seeing especially the children, since I got to work with as a pediatric dermatologist–I saw kids, struggling with psoriasis and, you know, it’s a visible condition, and so naturally you feel different from others and kids don’t know what it is, so you might get bullied and things like that. And so I think the reason why I love dermatology is the mental health aspect of it, because you know, how you look does matter when it comes to things like employment or just being likable. You know, it shouldn’t matter, but it does. And so, I hope that I can, help by separating the skin disease from those feelings.
Because when I read that Ted Grossbart book [Skin Deep: The Mind Body Program for Healthy Skin], he asked: What if your skin just went away? How would that change things for you?
It was an interview with a man he was helping. The man said, Oh, well then I guess I’d have to face my fear of talking to women. And Ted was like, Well, I want you to see that those are two separate things, and we can work on that second one. But the true answer would be, your life wouldn’t be different without your skin. [Your skin condition can be so tied to self-worth], it’s like we identify with it. It almost becomes an excuse to not do things, but it doesn’t have to be. I’m sure it was for me at one point, but now, when my skin gets better and if I don’t feel low, then it helps me remind myself that it doesn’t define me. I’m more than just whatever my skin wants to do. Sometimes it wants to be angry and red, and I’m just like, okay, it’s fine; I need to take care of myself.
It seems like it is one of those physical things that, like you said, because it’s visible to others, it gets conflated with identity or others’ perceptions of our identity. I’m teaching a course right now where we are looking at the history of Hansen’s disease, what used to be called leprosy, and for a long time it was even considered a sign of “sin” or moral failing. Because they didn’t understand it as an infectious disease and didn’t have a diagnostic test, it was just people who had a variety of visible skin problems being forcibly segregated, often for reasons of political oppression, so I feel like there is a social history to the stigmatization of skin disease.
Yeah, absolutely. And most people when they hear dermatology, they think cosmetics or Botox injections. However there’s so many facets to it. Like I mentioned, I’m going into pediatric dermatology but, you know, there’s like a huge range of applications like skin cancer and melanoma, you know there’s so much research into that, and complex medical dermatology, like helping patients with Lupus, the list goes on. It’s very exciting.
And I just love that it can expand [to include] like all the other specialties, almost; [a dermatologist is] like a detective. And then I remember in a personal statement when I was applying for residency,, I did write that our sense of self worth is really related to [our skin], how it shouldn’t be that way but it is. Anyway, I just hope I can continue to help lift people and [help them] not struggle.
I was curious how you feel your experience as a writing center tutor comes into play in your work in medicine.
You know, I didn’t realize until I remember talking to Vainis about it, and he said, more than ever, you know, with people texting, we’re writing the most we’ve ever written in the history of time. And so, in medicine, you have to be the historian for your patient when they are coming in, and so I think being able to write a very succinct “history of present illness”–[that’s the] medical term for it–is really important and then also having a good assessment and plan. Every note has a certain structure that everyone follows: Subjective, Objective, Assessment, and Plan. The subjective part is what the patient tells you; the objective is like their vital signs, what did you find on the physical exam; and then assessment is what do you think’s going on like, what’s on your differential, do they have heart failure, do they have a heart attack. And then your plan is like, okay, what are you gonna do to figure that out? And so, I was obsessive with my notes in the ICU– I’m very specific, like, these are the dosages, they take them this many times a day, versus when people just write “continue present management” or something, and I’m like, “Well, how many times a day? They didn’t put it in!” So it’s really great, I think, as a skill, as a bottom line is being able to communicate.
That’s the biggest thing in health care, you have to communicate well, otherwise it’s bad for patient care. Not only obviously to your peers and your colleagues, you know, the different consultants to the patient. With the patient’s family obviously there’s less writing and more talking. But I think as a tutor you’re talking with your peers, and you know, with the WC philosophy, in [222] I learned about like antiracism, feminism . . .and then also taking sociology courses really helped me to remove the biases that I may have. And so I think having awareness is something that I learned as a Writing Center tutor and that sometimes what the person on the other end needs is just for you to listen to them and work with them but not you giving your experience, like, oh yeah, like when I did this, I did that. Sometimes that’s helpful if they’re asking for it, but most times they just need some redirection.
And when families have to make difficult decisions about code status, or pulling the plug, you have to do it in a very careful manner. And, yeah, I feel like being a WC tutor, my experience to get to know your writer, like why are they writing this thing–it’s helpful. So if you’re talking to a family member, what’s important to them? Do they want everything done no matter if their quality of life is not so great? Yeah, in so many ways I can think of being a WC tutor translated into being a really great physician, and then, obviously, I think my writing got better when I worked with other writers. So then, having to write these descriptions or personal statements was so challenging but having that background helped me much better versus my peers who haven’t had as many English courses [and found it] much harder to really express themselves.